Unsafe Prescribing is a System Problem, (Not Just a Provider Problem)
Part 3 of 4: Learn how to pressure leadership to adopt clinic-wide policies for benzos, stimulants, Hypotics and opioids to protect your license.
When you inherit a high-risk patient panel, you are often being asked to solve a systems failure alone. Leadership knowingly allowed unsafe or out-of-scope prescribing to continue because it kept patients quiet and satisfied (even if it put them, and the clinic, at risk).
You are not just correcting unsafe care; you are swimming upstream against a culture that allowed this to form. This is why providers quickly burn out when they attempt to "clean up" a panel without structural backing.
1. You Cannot Fix This Alone: Demand Structural Backing
If your leadership won’t formally support guideline-based care, you are the one at legal risk, not them. You can only practice safely if you have explicit backing, ideally from the medical director, administration, and pharmacy leadership.
The problem is that you are being asked to enforce standards no one else has to follow—which makes you look like the unreasonable one.
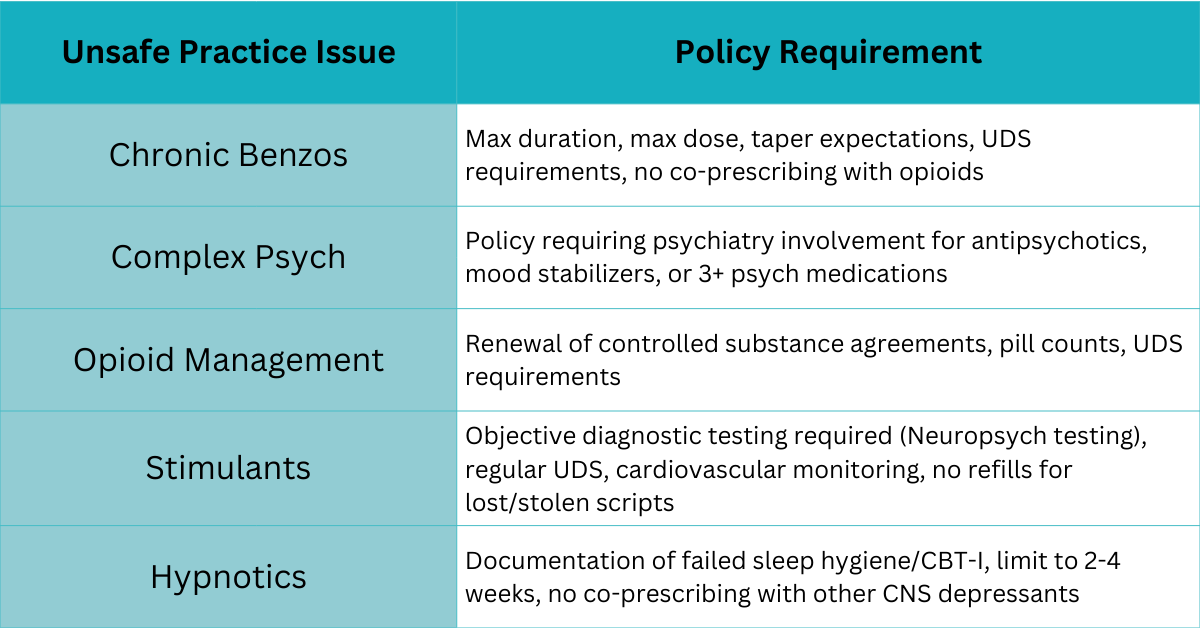
The Core Problem: Lack of Policy
Unsafe prescribing cultures only change when leadership formally adopts clinic-wide standards. Your boundaries must become clinic policy, not just your personal preference.
If policies do not exist, leadership must either: 1) Commit to them or 2) Accept the risk that unsafe prescribing will continue. That risk should not fall on your license.
2. Bring in Behavioral Health Early
The vast majority of patients on chronic, long-term benzodiazepines, stimulants, or hypnotics need behavioral health support to manage their underlying anxiety, ADHD, or insomnia. This is a critical clinical and legal step.
Proactive Referral: Even if you have to manage a taper yourself, you should document that you offered Cognitive Behavioral Therapy (CBT) and/or provided a clear referral for counseling.
It’s a Clinical Intervention: Frame the behavioral health referral as an essential step in the safe management of their condition, not just an optional add-on. For hypnotics, this includes documenting failed CBT-I before continuing long-term medication.
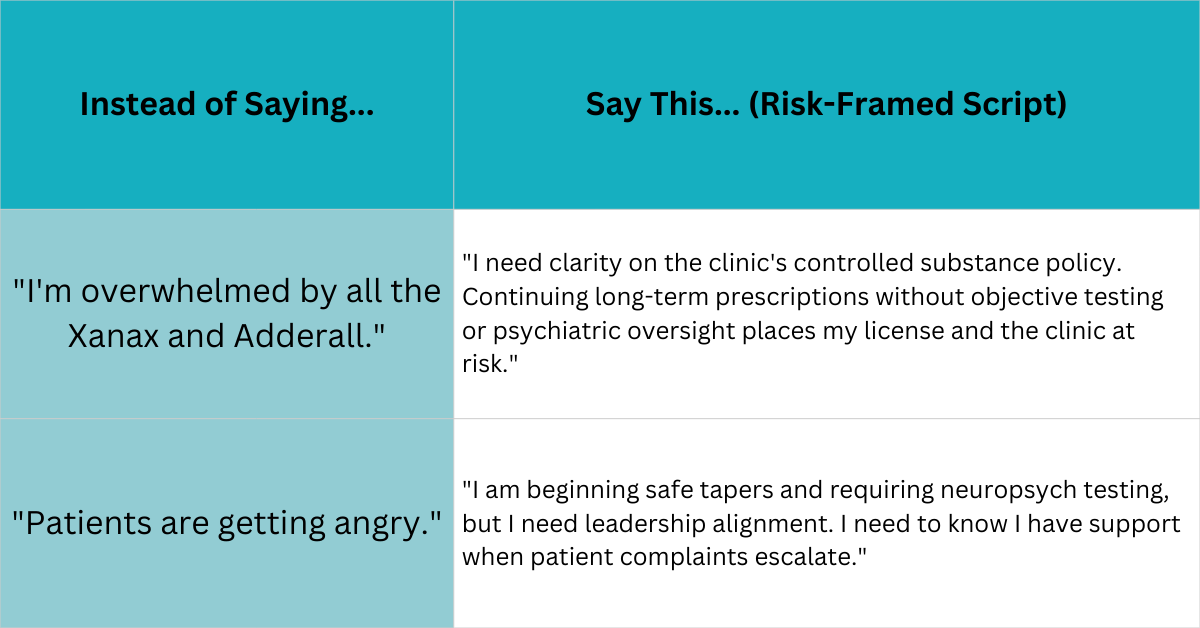
3. Talk to Leadership About Risk and Liability
Leaders respond to risk, not necessarily clinical nuance. If you need policy change, frame the conversation around the financial and legal liability the clinic is carrying by having NPs manage out-of-scope psychiatric or pain cases.
This approach turns the problem back to leadership where it belongs. If they ask you to continue unsafe prescribing, request that expectation in writing.
4. Decide Your Professional Alignment
You are allowed to conclude that the organizational values are not aligned with your professional ethics. You may decide that this clinic wants a refill machine, not a medical professional.
Leaving is not a failure; it is self-preservation. If you choose to stay, you must strategically shift from "fixing the system" to meticulously protecting yourself within it.
💡 Use Your Systems to Force Alignment and Protect Yourself
If your leadership is unsupportive, Chart Smart Mastery gives you the actionable, policy-driven tools to survive:
Module 7: Delegating & Collaborating: Learn the precise scripts to communicate and delegate non-urgent tasks to your team.
Module 8: Inbox & Administrative Tasks: Master the art of documenting patient barriers and transferring high-risk work to the appropriate specialist or leader.
Module 9: Charting for Quality & Compliance: Provides the ultimate checklist for documenting refusals, informed consent, and all patient communication to create an iron-clad legal defense.
👉 Enroll in Chart Smart Mastery
Read This Whole Series:
Part 1: When Inheriting a Patient Panel Means Inheriting Unsafe Prescribing
Part 2: When Safe Practice Makes You the “Difficult” Provider
Part 4: How to Leave a Toxic Practice (or Survive It) with Your Professional Identity Intact